Evaluation of Coagulation Complications and Global Assays in Acute Promyelocytic Leukemia (APL) by Jeffrey W. Taub, M.D., FAAP and Madhvi Rajpurkar, M.D., Co-Directors, Division of Hematology-Oncology
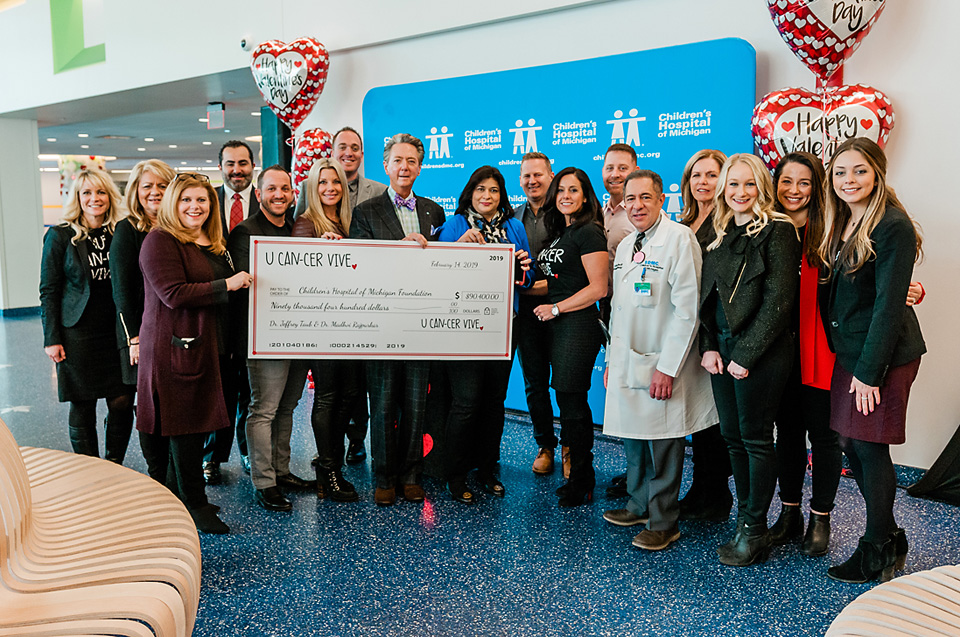
Funded Amount: $90,400
The U Can-Cer Vive Foundation recently made a grant to the Children’s Hospital of Michigan Foundation to support research in acute promyelocytic leukemia (APL) in children at the Children’s Hospital of Michigan. The U Can-Cer Vive Foundation’s partnership with the Children’s Hospital of Michigan Foundation provides vital funding for cancer research at the Children’s Hospital of Michigan to help create a cancer free world for children.
Cancer is the leading cause of death from disease for children in the United States. Every year, 15,780 young people are diagnosed with cancer, with leukemia and brain tumors as the most common types of pediatric cancer. Thanks to research, today about 85% of kids with the most common types of cancer will live. Unfortunately, progress has been limited for other types of cancer, and for some kids there is still little hope for a cure. For these children, developing new drugs and therapies is crucial. Unfortunately, few federal resources are targeted to developing treatments and cures for children with cancer. Funding from the U Can-Cer Vive Foundation will support this new cancer research study:
Evaluation of Coagulation Complications and Global Assays in Acute Promyelocytic Leukemia (APL) in Children
Funding Amount $90,400
Acute Promyelocytic Leukemia (APL) is an aggressive subtype of the cancer acute myeloid leukemia (AML). In APL, there are too many immature blood-forming cells (promyelocytes) in the blood and bone marrow. These immature cells are unable to function like healthy mature white cells. The accumulation of these immature promyelocytes leads to a shortage of normal white and red blood cells and platelets in the body. Because of this, a child with APL can suffer from potentially fatal episodes of bleeding and/or clotting in the brain, lungs, and other organs.
APL is highly curable, except that these severe bleeding or abnormally excessive clotting complications cause up to a third of affected children to die within the first month before their cancer treatments have a chance to work. Up until now, routinely performed coagulation tests have not been able to give physicians reliable information to predict which children are at risk for these devastating complications. This lack of information is a major barrier to improving the outcomes of this potentially curable yet deadly disease.
This project will study children with APL and use unique bleeding/clotting tests to better understand the causes of APL-related bleeding and clotting. These studies will help identify the children who are at highest risk of suffering these debilitating or deadly bleeding and clotting events in the hope that these complications can be controlled.
This study is being conducted in collaboration with the Children’s Oncology Group (COG), the largest clinical trial network for treating children with cancer in the United States. No individual institution can perform this type of research solely on their own local patients. Blood samples will be obtained from children enrolled in the COG APL clinical trial study at multiple participating medical centers in the United States as well as from Australia and New Zealand and will be shipped to the Special Coagulation Laboratory at the Children’s Hospital of Michigan.
In this study, researchers will evaluate novel biomarkers and tests that determine the total coagulation potential of blood in children with APL. The unique bleeding/clotting tests that will be performed in Special Coagulation Laboratory are not widely available and have never previously been performed on children with APL in COG trials. The Special Coagulation Laboratory is world-renowned for carrying out standard and advanced coagulation testing.

Jeffrey W. Taub, M.D, and Madhvi Rajpurkar, M.D, will collaborate on this study. Dr. Rajpurkar is the Division Chief of Hematology at Children’s Hospital of Michigan and Professor of Pediatrics at Wayne State University School of Medicine. She also is the Purcell-Lusher Endowed Chair for research in thrombosis and coagulation disorders in children. Dr. Rajpurkar has numerous peer-reviewed articles, serves on various national committees and is an international expert on pediatric bleeding and clotting issues. Dr. Taub is the Division Chief of Oncology at Children’s Hospital of Michigan and Professor of Pediatrics at Wayne State University School of Medicine. He currently holds the Ring Screw Textron Endowed Chair in Pediatric Cancer Research. As an authority in childhood cancer, Dr. Taub has published over 100 research papers in leading medical journals. Dr. Taub is a childhood survivor of Hodgkin’s disease who received part of his treatment at Children’s Hospital of Michigan.
Both physicians hope that the results of this study can be used to help save the lives of more children with APL by identifying children at risk for the worst outcomes. The study should help physicians to better utilize existing treatments and to develop preventive strategies to address these deadly bleeding and clotting complications in children with APL, so that they can successfully complete their cancer treatment.

Acute promyelocytic leukemia (APL) is an aggressive subtype of the cancer acute myeloid leukemia (AML). About 4 to 8 percent of all childhood AML is the APL subtype. In APL, there are too many immature blood-forming cells (promyelocytes) in the blood and bone marrow. These immature cells are unable to function like healthy mature white cells. The accumulation of these immature promyelocytes leads to a shortage of normal white and red blood cells and platelets in the body. This unique complication causes a child with APL’s bleeding and clotting system to become very unbalanced. This can lead to fatal episodes of bleeding and/or clotting in the brain, lungs, and other organs.
APL is highly curable except that up to a third of children may die within the first month before their cancer treatments have a chance to work, due to severe bleeding or abnormally excessive clotting. Up until now the routinely performed coagulation tests have not been able to give physicians reliable information to predict which children are at-risk for these devastating complications. This lack of information is a major barrier to improving the outcomes of this potentially curable yet deadly disease.